By Joyce Famakinwa
The Program of All-Inclusive Care for the Elderly (PACE) concept has gained significant business and policy momentum over the past several months, with recent research also highlighting just how successful programs were at avoiding COVID-19 deaths compared to other care settings.
Despite that traction and the model’s clear benefits, PACE still faces a long list of formidable growth barriers.
An alternative to nursing homes, PACE is a Medicare and Medicaid program that helps keep people in their communities. Oftentimes, programs are run out of community-based centers with the support of in-home care providers and their staff.
“Embedded in this model is that the PACE program also addresses the social determinants of health for the enrollees and wraps around this care with a very comprehensive interdisciplinary care team,” Jade Gong, founder and principal of consulting firm Jade Gong & Associates, told Home Health Care News.
At any particular time, 95% of PACE enrollees are living in the community, with about 5% in nursing homes, according to Robert Greenwood, senior vice president of public affairs at the National PACE Association.
“This is pretty remarkable, given that you have to be eligible for nursing home care before you can even enroll in PACE,” he told HHCN.
Based in Alexandria, Virginia, the National PACE Association is an industry advocacy group that focuses on federal and state policies to support the financial viability of the PACE model.
Broadly, the majority of PACE participants are eligible for both Medicare and Medicaid. PACE operators receive a set monthly payment for each participant. Typically, PACE is both payer and provider.
“Having a capitated payment really helps the PACE model because we’re able to emphasize providing primary and preventive care over the things that are really expensive, which are emergency room visits, hospital visits or permanent placement in a nursing home,” Greenwood said.
While the PACE model has been attracting interest over the past few years, the COVID-19 emergency played a major role in ramping up this attention, according to Gong.
“The model just performs so well under COVID,” she said. “There are many different kinds of providers — nonprofit, for-profit, housing — that are interested in PACE or relationships with PACE programs.”
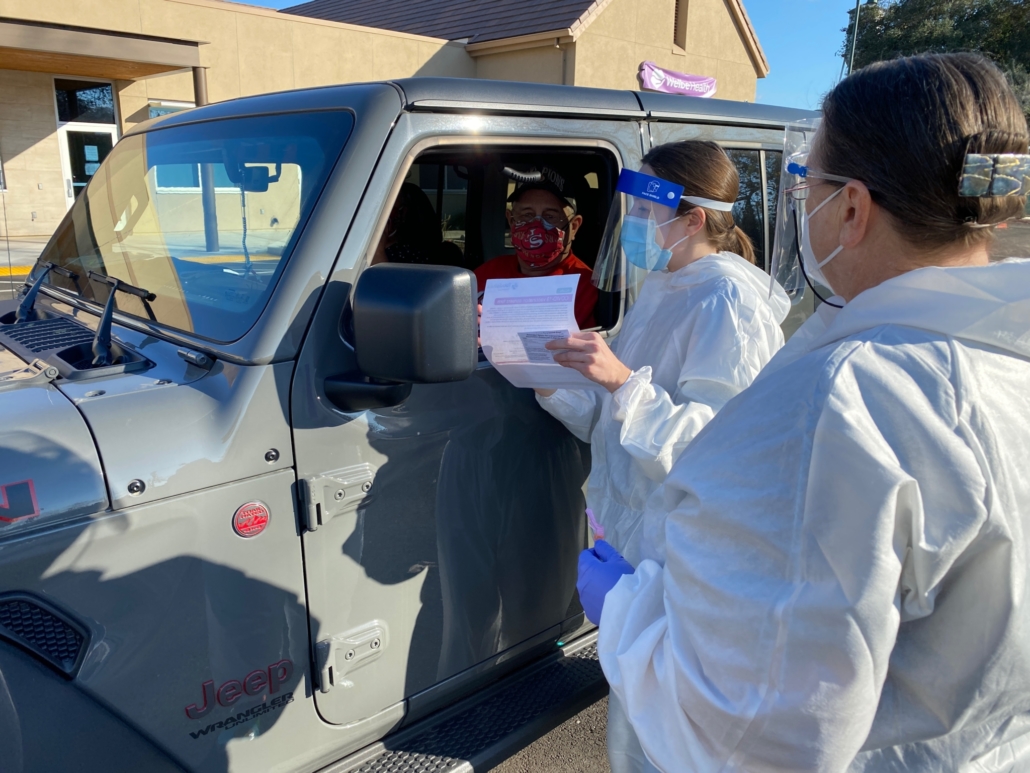
If one provider exemplifies the performance success the model saw amid the public health emergency, it’s WelbeHealth, a Menlo Park, California-based operator of PACE programs.
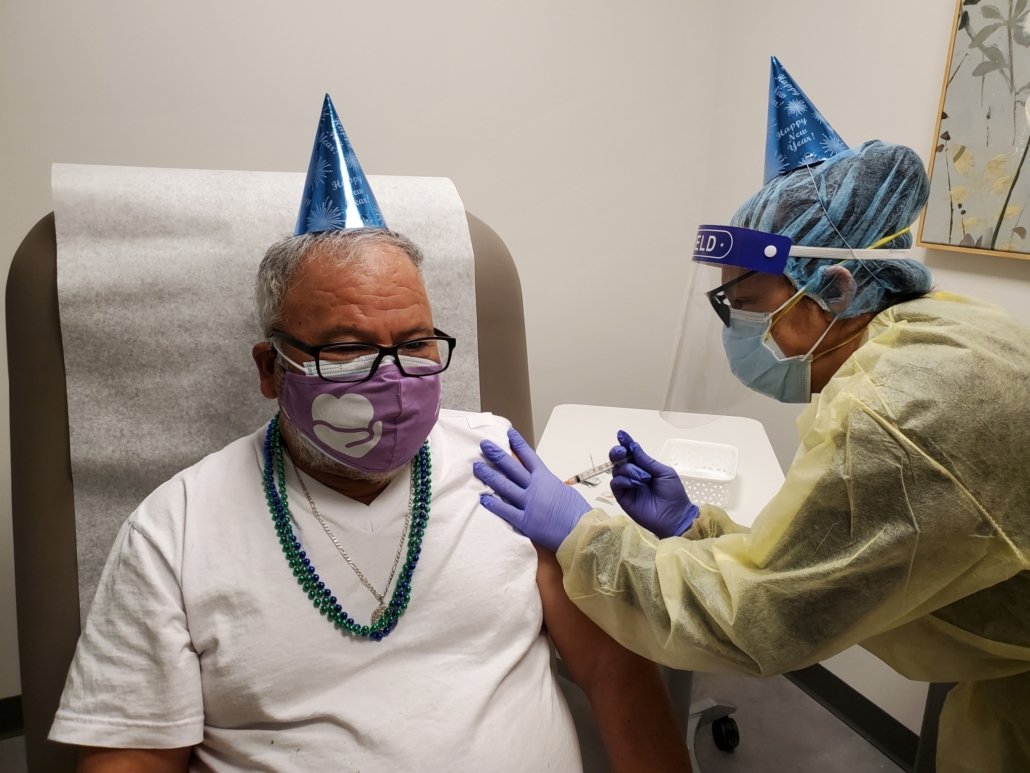
Overall, WelbeHealth and the PACE community had lower death rates than their nursing homes counterparts, research has found.
In fact, the national PACE COVID-19 death rate was 3.8%, compared to 11.8% in nursing homes. WelbeHealth’s COVID-19 death rate was 2.4%, according to a recent case study conducted by UC Berkeley.
For context, WelbeHealth serves LA and Central Valley, which have both been COVID-19 hotspots at times.
“These were places where crematoriums listed their pollution caps because they had too many bodies piling up,” Si France, founder and CEO of WelbeHealth, told HHCN. “This is where paramedics were asked to start rationing care. The hospitals were full, and they had to fill up their parking lot pop-up units. That was the nightmare context where we had these dramatically lower death rates.”
Over the years, WelbeHealth has seen growth as the organization aimed to serve underserved markets in California. The company added a Fresno program in late 2020 and will serve about 1,000 participants by the end of the year.
“We ranked California cities by highest unmet need, and started working on serving them, in order, beginning with Stockton and Pasadena in 2019, then Long Beach in 2020,” France said. “None of these communities had any PACE services despite having a high need. You had no access to this program that increases quality of life and length of life.”
France noted that PACE enrollees experience an 80% reduction in depression and generally have a higher life satisfaction. They also tend to live longer under the comprehensive and interdisciplinary care model.
Despite strong outcomes from many PACE providers, such as WelbeHealth, there is still room for expansion.
In total, there are 140 PACE organizations operating 272 PACE centers in 30 states, serving over 56,000 participants, according to the National PACE Association.
One of the major barriers to furthering PACE expansion is how high the cost of entry can be for new operators.
“When an organization wants to look at developing a PACE program, it’s not just building the center, hiring the staff, having the right information systems, and leasing or buying the vans to provide transportation,” Greenwood said. “Part of the startup costs is operating in those initial months when you don’t have a big enough enrollment to bring in the revenue that really covers all your expenses.”
Another roadblock is the PACE application process, which requires the state to develop a rate-setting methodology for anyone who’s a Medicaid eligible PACE enrollee. States must also agree to take on certain oversight responsibilities.
“One of the things that really stops a provider from being able to develop PACE is the willingness of the state they’re operating in to support that development,” Greenwood said.
In an effort to drive PACE expansion, Sen. Bob Casey, a Democrat from Pennsylvania and chairman of the Senate Special Committee on Aging, introduced the “PACE Plus Act” in April.
The legislation has received a warm reception from industry insiders for being comprehensive and attempting to cut through red tape.
“I have some sense of optimism that we’re going to get some real traction on the bill this year,” Gong said. “I have talked to some of the senators in states where I have clients, and there’s tremendous interest in seeing PACE expansion.”
If passed, the PACE Plus Act would make room for the creation of new PACE programs and the expansion of current ones through federal grants. The legislation also encourages non-PACE states to take up the model by providing incentives.
Additionally, the legislation would lessen the bureaucratic burden that growing PACE programs face while also providing technical assistance resources.
Another bright spot has been various states’ willingness to consider the PACE model, according to Greenwood.
“States have been looking more closely at how they want to provide long-term care supports and services in the future,” he said. “They’re looking at what else they can do beyond offering nursing home residential care. I think they’ve become a lot more open to supporting PACE as a way to provide more healthy community-based services.”