WelbeHealth Becomes First Program of All-Inclusive Care for the Elderly (PACE) Provider to Convert to Public Benefit Company Status
FOR RELEASE: IMMEDIATE
DATE: 6/29/2022
WelbeHealth Becomes First Program of All-Inclusive Care for the Elderly (PACE) Provider to Convert to Public Benefit Company Status
MENLO PARK, CALIF.— Physician-led healthcare organization WelbeHealth recently became the first Program of All-Inclusive Care for the Elderly (PACE) provider to convert to a public benefit company (PBC).
Founded in 2015, WelbeHealth is a leading California PACE provider. An alternative to nursing homes, PACE is a Medicare and Medicaid program that helps keep people in their communities. WelbeHealth provides comprehensive home-based medical and social services to vulnerable seniors across California, including the cities of Stockton, Modesto, Pasadena, Burbank, Long Beach and Fresno.
In joining other companies that have become public benefit companies, including Patagonia, Seventh Generation and Vital Farms, WelbeHealth is exemplifying its commitment to helping seniors thrive and live longer, said WelbeHealth co-founder and CEO Si France, M.D.
“The seniors we serve are the elders of their communities and families,” Dr. France said. “By helping them thrive, they can live longer lives with greater connection, vitality and meaning. We’re converting to a public benefit company to ensure that our mission and purpose are protected for generations to come.”
Public benefit companies are obligated to take into consideration the concerns of all stakeholders, not just shareholders, prioritizing corporate responsibility and sustainability. For WelbeHealth, this means participants, their families and caregivers, employees, and the broader community.
“Both our independent board and management team wanted to formalize WelbeHealth’s commitment to its mission, clinical quality and positive community impact,” said WelbeHealth Board of Directors member Robert Margolis, M.D., founder of the Duke-Margolis Center for Health Policy. “By converting to a public benefit company, WelbeHealth is demonstrating its commitment to operating responsibly, sustainably and in the interest of all stakeholders, both now and in the future.”
This commitment to the greater good is not new. In fact, WelbeHealth was lauded for its elder care during the pandemic. A case study conducted by UC Berkeley found that WelbeHealth had a death rate more than 1.5 times lower than other PACE organizations and almost five times lower than nursing homes while, despite serving patients in some of California’s most impacted counties.
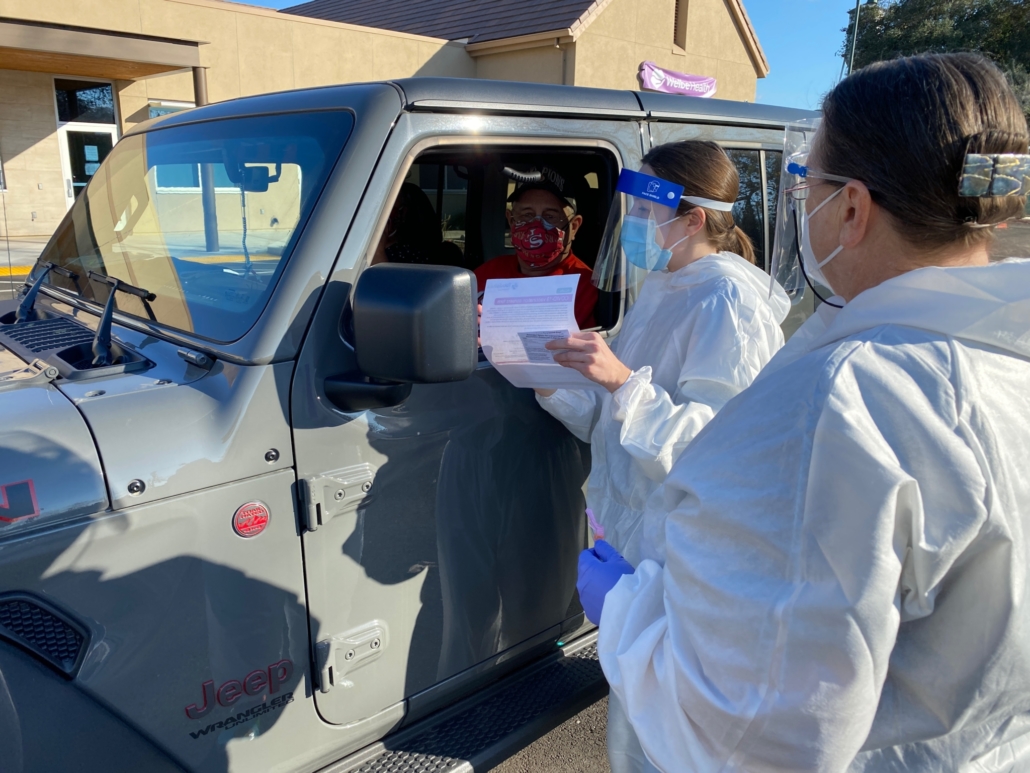
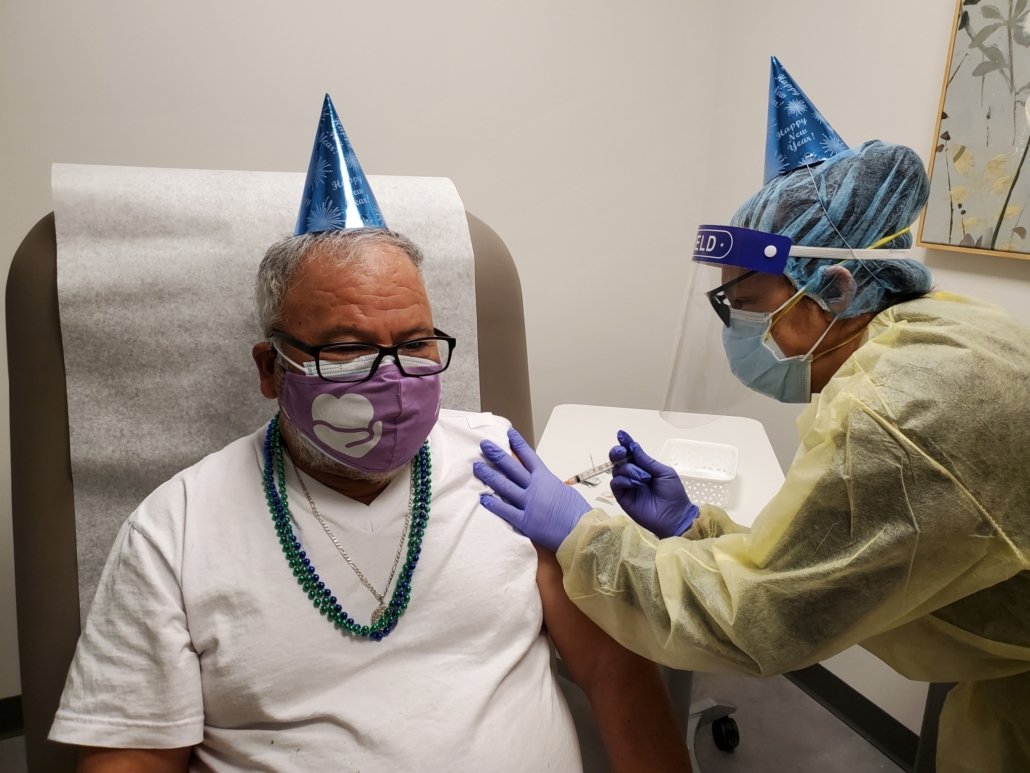
“As the pandemic came in waves, WelbeHealth mobilized not only to vaccinate its own participants but to also vaccinate thousands in the greater community, which had an exponential impact on saving lives,” Dr. France said. “We want to take full responsibility for our part in making the world a more compassionate, loving place.”
About WelbeHealth
Founded in 2015, WelbeHealth is a physician-led organization that coordinates senior care, including all medical and dental care, physical and occupational therapy, transportation to medical appointments, meals and personal care services. WelbeHealth teams close the loop on comprehensive care to keep the most vulnerable seniors living safely in their own homes. WelbeHealth delivers these services through the Program of All-Inclusive Care for the Elderly (PACE), a Medicare and Medicaid program. WelbeHealth operates four programs in California: Stockton/Modesto, Pasadena/Burbank, Long Beach and Fresno. For more information, please visit welbehealth.com.