Courage to love: Realizing a future without nursing homes
Three alums reunite to improve the lives of the frailest and most vulnerable senior citizens through participation in a U.S. health care program.
– When Si France, M.D. (SVO 08-12), Vaneesh Soni, M.D. (DET, DBI, SCA 99-15), and Matt Patterson, M.D. (SVO 09-12) first met, they were streamlining hospitals. “At McKinsey, we were these three doctors who wanted to do good value-based care,” says Si.
They reunited to do just that by founding WelbeHealth, which enables frail and elderly senior citizens to continue living in their homes and communities through participation in a U.S. government program known as PACE (Program of All-Inclusive Care for the Elderly).
Matt, who grew up in a Navy family and became a doctor for the Navy SEALs, is Welbe’s President and clinical operations leader. Vaneesh is the team’s resident strategist and Chief Growth Officer, driving Welbe’s mission-driven expansion. Si is the out-of-the-box entrepreneur who has co-founded two health care startups and is leading Welbe as the CEO. Armed with complementary leadership profiles, an interdisciplinary team, and a shared values system, Welbe aspires to realize a future where seniors can receive dynamic care without the need for nursing homes.
We sat down with the trio to discuss Welbe’s care services, purpose-driven culture, and their response to the COVID pandemic, which saw them at the center of one of the hottest infection zones in the world.
Tell us about Welbe’s culture.
Vaneesh: We invest as much energy into organizational health and culture as our strategy and business model. We don’t want to be a company with the best strategy but have poor performance overall because we have a toxic culture. Service to seniors is our common intent, and clinical quality is our North Star. Our growth rate is tied to the pace at which we can ensure consistent, high-quality care.

Si: We started the company to create a culture based on a mission and values system different from what is more traditional in Silicon Valley. We knew that it would take courage to build a values-based company and that we would need to view our patients through the eyes of their loved ones. We called this our “courage to love” culture, and it permeates everything we do, whether we’re interacting with our team or interacting with our patients.
Matt: Our core values of courage to love, pioneering spirit, and shared intention are the unquestioned foundation for ensuring that we have healthy teams, our people feel uniquely cared for, and we serve vulnerable seniors with a commitment to clinical excellence. What excites me is that we’re bringing consciousness and love as a priority within our business model. We want to normalize individuals being able to show up as their authentic selves and engage at that level with each other and those that they serve.
Tell us about Welbe’s care model. What distinguishes it from other services?
Si: Our care model is called “PACE,” Program of All-Inclusive Care for the Elderly. We provide 24/7 medical and social services to frail seniors to stay healthy, live at home, and stay out of a nursing home. When people enroll in PACE, their life expectancy goes up by one-third, clinical scores improve, and it even saves taxpayers $10,000 per patient annually.
Vaneesh: PACE has an 80% reduction on depression scores nationally. As both the health plan and the provider of services, we emphasize the social and the human components of care. We can greenlight things that are truly in the best interest of each participant, medically, socially, as well as things that bring joy in life.
Matt: PACE has been around for decades, but we’re changing the landscape by bringing these services and outcomes to those who would otherwise not have them, in areas of the country that are in significant need, and at a speed and scale that previously has never been done before.
How did Welbe respond during the pandemic?
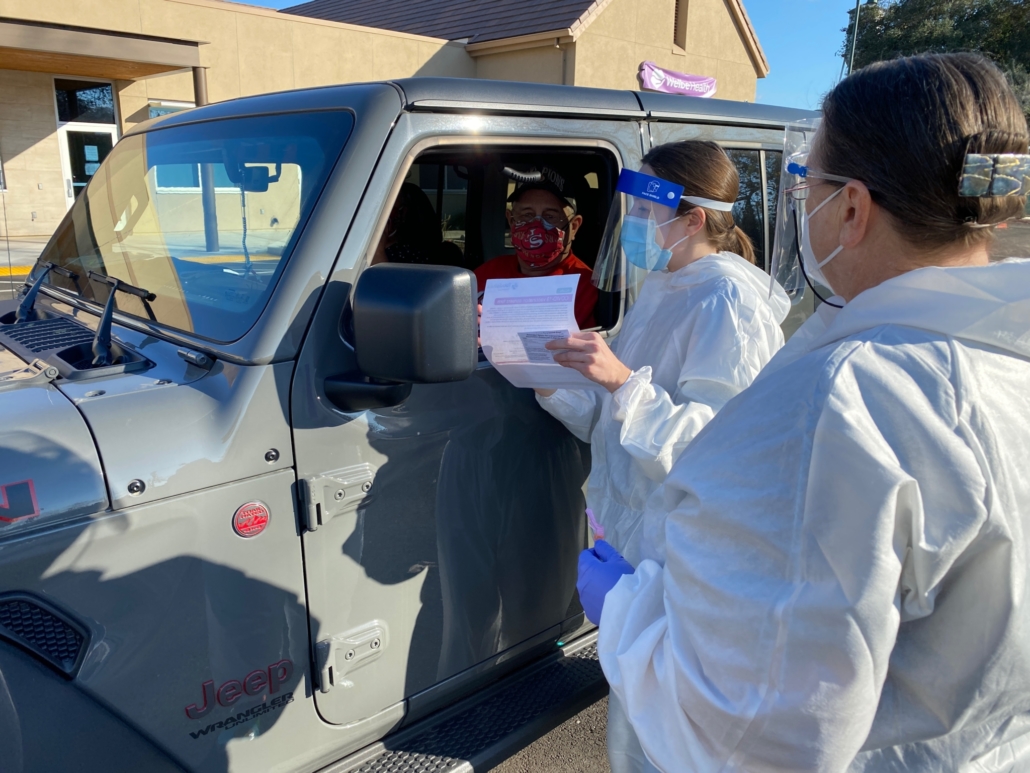
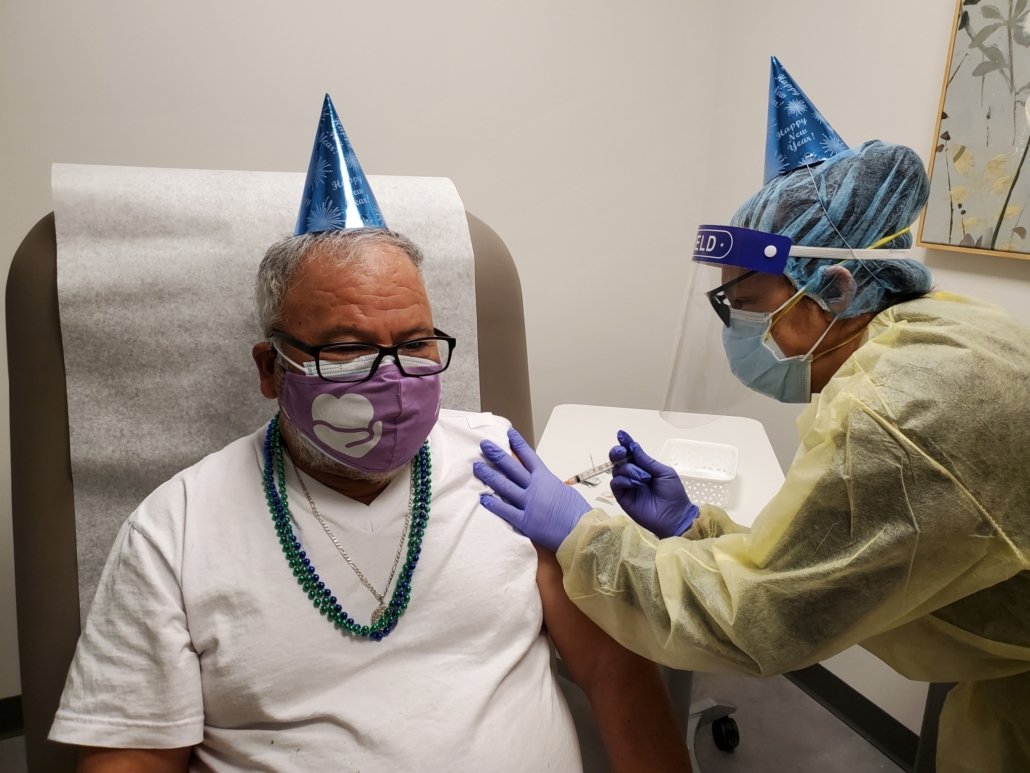
Si: We’re the first organization to do bubble-style testing, where our nurses would take a COVID test before entering anyone’s home. We were the first non-hospital owned program of our kind to vaccinate all of our team and patients. We also partnered with counties across California and vaccinated 2,000 frail seniors and front-line health care workers in the community who had nothing to do with Welbe.
Vaneesh: We closed our centers two weeks before the state of California announced the lockdown. Within four days of the lockdown, we had deployed a tablet-based, home-and-remote care model. I think the proudest moment was helping rescue seniors out of nursing homes. Many seniors in nursing homes don’t require 24/7 care; they are in a nursing home because they don’t have access to stable housing. We partnered with housing institutions to find them stable and safe housing, and provided care for them in those environments.
Matt: In the first year of the pandemic, COVID-19 mortality rates for nursing home individuals were upwards of 14%. The U.S. national average of PACE programs was about a third less, and Welbe was about a 10th. Our outcomes were 10x better than nursing home environments, and we were in two of the hottest areas for COVID infection in the entire world at various points. It’s a testament to the fact that we were very bold and decisive in deploying technology enablement, best-in-class rapid testing, early adoption of vaccination, and mass administration of vaccinations.
What impact did McKinsey have on you?
Matt: It was a profound tipping point in my journey, not the least for which I met two of my greatest friends in Si and Vaneesh. McKinsey also introduced me to the effectiveness of the remote working model by showing that I can have a laptop and work from anywhere in the world. Welbe’s technology footprint was built around a similar remote model that allowed us to be well-positioned and decisive during the pandemic.
Vaneesh: We rely on our McKinsey experiences or problem-solving daily. McKinsey showed me that it’s possible to deliver amazing impact and still do well financially and grow. Through different engagements and geographies, I gained exposure to different health systems and clinical models.
Si: It’s impossible to underestimate McKinsey’s impact on my career, from relationships, to learning how to build a principles-driven organization and how to think and communicate effectively. McKinsey gave me the tools to serve on a macro level. It was the best career decision I could have made to launch my career.
What does Welbe’s mission mean to you?
Si: What it means for me is a force for good in the world. Through the work we do and through our culture, we are caring for people beyond ourselves. To give an example, we had a patient who lived at home alone with her dog. She fell, broke her pelvis, was in the hospital, and as she recovered, she got a call from the local shelter saying, “Your neighbors reported an abandoned dog. We’re going to need to put it down.” She called our licensed vocational nurse at the center, and our LVN went down and rescued the dog and found a place for it while she recovered. Our patient said that the minute she learned of the rescue, she started going to physical therapy to get better as quickly as possible and get home to her dog.
Matt: My mom is a vulnerable senior with chronic mental illness. I have seen the failures of traditional health care models in senior care. What WelbeHealth’s mission means for me is that we advocate for those in our culture who are at the wrong intersection of not being valued and most at risk. It’s individuals who have very little social capital who are being left behind. Through our service, they can experience and share the love and wisdom that they have within them and have gained over their lifetime.
Vaneesh: What it means for me is service. In the Indian culture, we have different phases of our life: a phase for education, a phase for building a family, a phase for working, so on. There’s also a phase for service to others – called Seva.
Welbe is our service to our seniors. Our seniors, especially in the Indian culture, have the most wisdom and should be the most revered. When Matt, Si, and I reunited after McKinsey, we determined that Welbe would be governed by a profound sense of purpose to serve the most frail and vulnerable seniors and ensure they are embraced and cared for with dignity and respect so that they can age gracefully in the community or their own homes.
(This article is published in the McKinsey Alumni Center here.)